· Updated: · GoodSleep Team · science-of-sleep · 12 min read
The Connection Between Sleep and Mental Health: A Comprehensive Guide
Introduction
The relationship between sleep and mental health is one of the most significant—and often underappreciated—connections in human health. For decades, sleep problems were viewed primarily as symptoms of mental health conditions. Today, research reveals a far more complex picture: sleep and mental health influence each other in profound, bidirectional ways.
Poor sleep can trigger or worsen mental health problems. Mental health conditions can disrupt sleep. This creates a cycle that can be difficult to break—but understanding the science behind this relationship is the first step toward reclaiming both restful nights and emotional well-being.
The Science Behind Sleep and Mental Health
What Happens to Your Brain During Sleep
Sleep isn’t passive downtime. It’s an active period during which your brain performs essential maintenance and processing that directly impacts mental health:
During NREM (Non-REM) Sleep:
- The brain clears metabolic waste products through the glymphatic system
- Stress hormones like cortisol decrease to baseline levels
- Neural connections are strengthened or pruned based on the day’s learning
- Growth hormone is released, supporting tissue repair and regeneration
During REM Sleep:
- The brain processes emotional experiences from the day
- Emotional memories are consolidated and integrated
- The amygdala (the brain’s emotional center) is highly active
- Neurotransmitter levels are rebalanced
For a deeper understanding of these stages, see our Ultimate Guide to Sleep Cycles.
The Neuroscience of Sleep and Emotion
Several key brain systems link sleep and mental health:
The Prefrontal Cortex
The prefrontal cortex—responsible for rational thinking, impulse control, and emotional regulation—is highly sensitive to sleep deprivation. Studies using functional MRI have shown that after just one night of poor sleep, the prefrontal cortex shows significantly reduced activity, while the amygdala becomes hyperreactive.
This means sleep-deprived people:
- React more strongly to negative stimuli
- Have difficulty calming emotional responses
- Make poorer decisions when emotionally aroused
- Show decreased ability to recognize positive experiences
The Amygdala and Limbic System
Research by Matthew Walker at UC Berkeley found that after 35 hours of sleep deprivation, the amygdala showed a 60% increase in reactivity to negative emotional images compared to well-rested participants. The connection between the amygdala and prefrontal cortex was also weakened, explaining the loss of emotional control.
Neurotransmitter Systems
Sleep affects the balance of critical neurotransmitters:
| Neurotransmitter | Role in Mental Health | Effect of Sleep Deprivation |
|---|---|---|
| Serotonin | Mood regulation, well-being | Decreased production and sensitivity |
| Dopamine | Motivation, pleasure, reward | Disrupted signaling, impaired reward processing |
| GABA | Calming, anxiety reduction | Reduced effectiveness |
| Norepinephrine | Alertness, stress response | Dysregulated, contributing to anxiety |
The HPA Axis and Stress Response
The hypothalamic-pituitary-adrenal (HPA) axis controls your body’s stress response. Sleep deprivation dysregulates this system:
- Elevated cortisol: Sleep-deprived individuals show higher evening cortisol levels (when cortisol should be lowest)
- Blunted cortisol awakening response: The natural morning cortisol surge is diminished
- Prolonged stress recovery: It takes longer to return to baseline after stressful events
- Increased inflammation: Sleep deprivation elevates inflammatory markers linked to depression
The Impact of Poor Sleep on Mental Health
Chronic sleep deprivation or poor sleep quality creates cascading effects on mental well-being:
Cognitive Effects
- Impaired concentration and attention: Difficulty focusing on tasks
- Memory problems: Both encoding new memories and retrieving existing ones
- Reduced problem-solving ability: Decreased cognitive flexibility
- Slowed processing speed: Taking longer to understand and respond
- Poor judgment: Difficulty evaluating risks and making decisions
Emotional Effects
- Increased irritability: Shorter temper, more reactive to minor frustrations
- Heightened anxiety: Exaggerated worry and nervous tension
- Depressed mood: Feelings of sadness, hopelessness, or emptiness
- Emotional instability: Rapid mood swings and difficulty regulating emotions
- Reduced resilience: Less able to bounce back from setbacks
Behavioral Effects
- Social withdrawal: Decreased desire for social interaction
- Decreased motivation: Difficulty initiating activities
- Increased substance use: Using caffeine, alcohol, or other substances to cope
- Reduced physical activity: Feeling too tired to exercise
- Changes in eating patterns: Often increased appetite for high-calorie foods
Common Mental Health Conditions Related to Sleep
Depression and Sleep
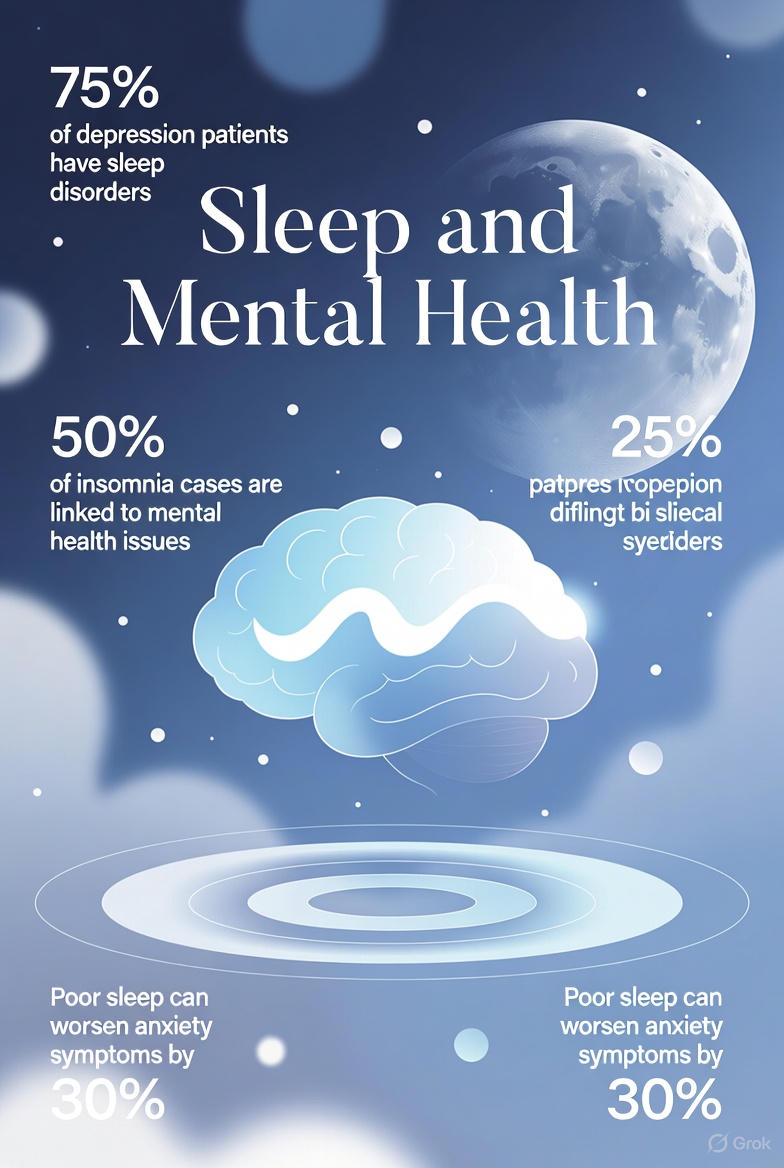
The relationship between depression and sleep is perhaps the most extensively studied. Approximately 75% of people with depression experience sleep problems, including:
Insomnia in Depression:
- Difficulty falling asleep due to rumination
- Early morning awakening (waking hours before intended)
- Fragmented sleep with multiple awakenings
- Non-restorative sleep despite adequate duration
Hypersomnia in Depression:
- Sleeping 10+ hours but still feeling tired
- Difficulty waking up
- Excessive daytime sleepiness
- Using sleep as escape from negative feelings
The Bidirectional Relationship:
Research shows this isn’t simply a one-way street:
- People with insomnia are 10 times more likely to develop depression
- Treating insomnia can significantly improve depression outcomes
- Sleep disturbance often precedes depressive episodes
- Sleep problems that persist after depression treatment predict relapse
Sleep Architecture Changes in Depression:
Studies show people with depression often have:
- Shorter time to first REM period (reduced REM latency)
- Increased REM density (more rapid eye movements during REM)
- Reduced slow-wave (deep) sleep
- More sleep fragmentation
Anxiety and Sleep
Anxiety disorders and sleep problems are intimately connected. The hyperaroused state that characterizes anxiety is fundamentally incompatible with the relaxation needed for sleep.
How Anxiety Disrupts Sleep:
- Racing thoughts: The mind won’t quiet down at bedtime
- Physical tension: Muscle tension, rapid heartbeat, shallow breathing
- Hypervigilance: Being too alert to external sounds or internal sensations
- Sleep-related worry: Anxiety about not being able to sleep (paradoxically worsening sleep)
- Nightmares and disturbing dreams: Processing anxiety during REM sleep
Specific Anxiety Disorders and Sleep:
| Disorder | Common Sleep Problems |
|---|---|
| Generalized Anxiety Disorder | Difficulty falling asleep, restless sleep |
| Panic Disorder | Nocturnal panic attacks, fear of sleep |
| Social Anxiety | Pre-event insomnia, rumination at night |
| PTSD | Nightmares, hypervigilance, sleep avoidance |
| OCD | Bedtime rituals prolonging sleep onset |
The Anxiety-Insomnia Cycle:
- Anxiety causes difficulty sleeping
- Poor sleep increases next-day anxiety
- Worry about sleep creates performance anxiety about sleeping
- Increased anxiety further disrupts sleep
- The cycle intensifies over time
Stress and Sleep
While stress isn’t a mental health diagnosis, chronic stress significantly impacts both sleep and mental health.
Acute Stress:
- Activates the sympathetic nervous system (“fight or flight”)
- Releases cortisol and adrenaline
- Increases alertness—useful for immediate threats, harmful for sleep
- May cause temporary sleep difficulties that resolve when stress passes
Chronic Stress:
- Persistently elevated cortisol disrupts circadian rhythms
- Creates a state of perpetual arousal
- Depletes neurotransmitter reserves
- Increases risk of developing anxiety and depression
- Causes lasting changes to sleep architecture
Occupational and Life Stress:
- Work-related stress: Deadline pressure, conflict, job insecurity
- Financial stress: Worry about money, debt, economic uncertainty
- Relationship stress: Conflict, caregiving responsibilities, loneliness
- Health stress: Chronic illness, medical procedures, health anxiety
- Major life events: Grief, divorce, moving, having children
Bipolar Disorder and Sleep
Sleep disturbances are particularly significant in bipolar disorder:
During Manic Episodes:
- Dramatically reduced need for sleep (feeling rested after 2-3 hours)
- Sleep deprivation can trigger manic episodes
- Racing thoughts prevent sleep onset
- Increased energy makes lying still difficult
During Depressive Episodes:
- Hypersomnia or insomnia
- Difficulty getting out of bed
- Non-restorative sleep
- Disrupted sleep-wake schedule
Stabilizing Sleep:
For people with bipolar disorder, maintaining consistent sleep patterns is often crucial for preventing mood episodes. Sleep deprivation—even from positive events like travel or celebrations—can trigger mania.
PTSD and Sleep
Post-traumatic stress disorder has a particularly complex relationship with sleep:
- Nightmares: Recurring traumatic dreams disrupt sleep and cause avoidance
- Hyperarousal: Difficulty feeling safe enough to sleep
- Sleep avoidance: Fear of nightmares leads to delaying sleep
- Fragmented sleep: Multiple awakenings throughout the night
- Obstructive sleep apnea: Surprisingly common in PTSD, possibly due to weight gain from medications or reduced physical activity
Breaking the Sleep-Mental Health Cycle
The bidirectional nature of sleep and mental health means that improving either one can benefit the other. Here are evidence-based approaches:
1. Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I is the first-line treatment for chronic insomnia, recommended before medication by the American Academy of Sleep Medicine. It’s particularly effective for people with comorbid mental health conditions.
Components of CBT-I:
Sleep Restriction Therapy:
- Temporarily limit time in bed to match actual sleep time
- Builds sleep drive and consolidates sleep
- Gradually extends sleep window as efficiency improves
Stimulus Control:
- Use the bed only for sleep and intimacy
- Leave the bedroom if unable to sleep after 15-20 minutes
- Return only when sleepy
- Wake at the same time every day regardless of sleep quality
Cognitive Restructuring:
- Identify and challenge unhelpful beliefs about sleep
- Replace catastrophizing thoughts with balanced perspectives
- Reduce performance anxiety about sleeping
Sleep Hygiene Education:
- Consistent sleep-wake times
- Optimal bedroom environment
- Limiting caffeine, alcohol, and screens before bed
Relaxation Training:
- Progressive muscle relaxation
- Deep breathing exercises
- Guided imagery
Research on CBT-I:
- 70-80% of patients show significant improvement
- Effects are maintained long-term (often better than medication)
- Also improves symptoms of depression and anxiety
- Can be delivered in-person, in groups, or via digital programs
2. Sleep Hygiene Practices
While sleep hygiene alone rarely cures insomnia, it provides a foundation for healthy sleep:
Timing:
- Go to bed and wake up at consistent times
- Avoid sleeping in more than 1 hour on weekends
- Limit naps to 20-30 minutes before 3 PM
Environment:
- Keep the bedroom cool (65-68°F / 18-20°C)
- Ensure complete darkness or use a sleep mask
- Minimize noise or use white noise
- Reserve the bed for sleep and intimacy only
Pre-Sleep Routine:
- Begin winding down 1-2 hours before bed
- Dim lights to signal melatonin production
- Avoid screens or use blue light blocking
- Engage in calming activities (reading, gentle stretching, bath)
Substances:
- Avoid caffeine after noon (or earlier if sensitive)
- Limit alcohol, which disrupts sleep architecture
- Be mindful of medications that affect sleep
3. Emotional Regulation Strategies
Building emotional regulation skills supports both sleep and mental health:
Worry Journaling:
- Write down concerns 1-2 hours before bed
- Problem-solve what you can
- Acknowledge what’s outside your control
- “Close” the journal to symbolically set aside worries
Mindfulness and Meditation:
- Regular mindfulness practice reduces rumination
- Body scan meditation promotes physical relaxation
- Mindfulness-Based Stress Reduction (MBSR) has strong evidence
- Apps like Headspace, Calm, or Insight Timer can guide practice
Progressive Muscle Relaxation:
- Systematically tense and release muscle groups
- Reduces physical tension associated with anxiety
- Can be practiced in bed as part of sleep onset routine
Gratitude Practice:
- Write down 3 things you’re grateful for before bed
- Shifts focus from problems to positives
- Associated with better sleep quality and mood
4. Cognitive Restructuring for Sleep Anxiety
Many people with insomnia develop anxiety about sleep itself. Common unhelpful thoughts include:
| Unhelpful Thought | Balanced Alternative |
|---|---|
| ”I must get 8 hours or I’ll be useless tomorrow" | "I can function even if my sleep isn’t perfect" |
| "I’ll never sleep well again" | "Sleep problems are common and treatable" |
| "I should be able to sleep—what’s wrong with me?" | "Many people struggle with sleep; this isn’t a character flaw" |
| "One bad night will ruin my whole week" | "My body can recover from occasional poor sleep” |
5. Addressing Underlying Mental Health Conditions
Sometimes improving sleep requires addressing the underlying mental health condition:
Therapy Options:
- Cognitive Behavioral Therapy (CBT) for depression and anxiety
- Acceptance and Commitment Therapy (ACT)
- Dialectical Behavior Therapy (DBT) for emotion regulation
- Eye Movement Desensitization and Reprocessing (EMDR) for PTSD
Medication Considerations:
- Some psychiatric medications help sleep (e.g., mirtazapine, trazodone)
- Some may disrupt sleep (e.g., certain SSRIs, stimulants)
- Work with your prescriber to optimize timing and selection
- Avoid long-term use of benzodiazepines or Z-drugs for sleep
Specific Strategies for Common Conditions
For Anxiety
Before Bed:
- Practice the 4-7-8 breathing technique (inhale 4 seconds, hold 7, exhale 8)
- Do a body scan to release physical tension
- Use guided imagery of a peaceful place
- Keep a “worry box” by your bed for thoughts that arise
During the Day:
- Regular exercise (but not within 3 hours of bedtime)
- Limit caffeine, especially after noon
- Practice mindfulness to reduce baseline anxiety
- Challenge anxious thoughts using CBT techniques
Environmental:
- Create a cool, dark, quiet sleep space
- Consider a weighted blanket (shown to reduce anxiety)
- Use calming scents like lavender
- Have a consistent, calming bedtime routine
For Depression
Morning Strategies:
- Get bright light exposure within 30 minutes of waking
- Open curtains or use a light therapy box
- Maintain a consistent wake time even when motivation is low
- Engage in light movement or stretching
During the Day:
- Schedule pleasant activities (behavioral activation)
- Get outside for natural light and gentle exercise
- Limit daytime napping to prevent nighttime insomnia
- Stay socially connected even when withdrawn
Evening Strategies:
- Avoid oversleeping—keep a consistent bedtime
- Create a routine that includes small pleasures
- Practice gratitude or positive reflection
- Avoid alcohol as a sleep aid (it worsens depression and sleep)
For Stress Management
Establish Boundaries:
- Create a cutoff time for work (no checking email after 8 PM)
- Have a “shutdown” ritual to end the workday
- Keep work materials out of the bedroom
- Learn to say no to excessive commitments
Process the Day:
- Do a brief “brain dump” earlier in the evening
- Review the day’s accomplishments
- Plan tomorrow’s priorities (to prevent bedtime planning)
- Practice letting go of unfinished tasks until tomorrow
Build Stress Resilience:
- Regular exercise
- Social support and connection
- Hobbies and activities that provide flow states
- Time in nature
When to Seek Professional Help
Consider consulting a healthcare provider if:
Warning Signs
- Sleep problems persist for more than 2-3 weeks
- You experience severe anxiety about sleep
- Mental health symptoms significantly impact daily functioning
- You’re using alcohol or substances to sleep
- You have thoughts of self-harm or suicide
- Home strategies haven’t helped after consistent effort
Types of Professionals Who Can Help
Primary Care Physician:
- Initial assessment and ruling out medical causes
- Referrals to specialists
- Medication management if appropriate
Sleep Specialist:
- Evaluation for sleep disorders (sleep apnea, restless legs, etc.)
- Sleep studies when indicated
- Specialized treatment for complex cases
Psychiatrist:
- Medication management for mental health conditions
- Complex cases involving multiple conditions
- When mental health symptoms are severe
Psychologist or Therapist:
- CBT-I for insomnia
- Therapy for anxiety, depression, trauma
- Ongoing support and skill building
Building a Supportive Sleep Environment for Mental Wellness
Physical Environment
Optimize Your Bedroom:
- Temperature: 65-68°F (18-20°C)
- Darkness: Blackout curtains or sleep mask
- Quiet: Earplugs, white noise machine, or fan
- Comfortable bedding appropriate for the season
- Remove or cover electronics with standby lights
Air Quality:
- Consider an air purifier if allergies affect sleep
- Keep windows open when weather permits
- Add plants that improve air quality
Declutter:
- A messy room can increase stress and anxiety
- Keep the bedroom minimal and calming
- Remove work materials and electronics
Mental and Emotional Environment
Create Psychological Safety:
- The bedroom should feel like a refuge
- Address relationship conflicts before bed when possible
- Make the bedroom a “worry-free zone”
Establish Rituals:
- Consistent wind-down routine signals sleep to the brain
- Include activities that promote calm (not screens)
- The routine itself becomes a cue for relaxation
Positive Associations:
- Reserve the bed for sleep and intimacy only
- Don’t watch TV, work, or scroll in bed
- If you can’t sleep, leave the bedroom temporarily
The Role of Exercise in Sleep and Mental Health
Physical activity is one of the most powerful tools for improving both sleep and mental health:
Benefits for Sleep
- Reduces time to fall asleep
- Increases slow-wave (deep) sleep
- Improves sleep efficiency
- Helps regulate circadian rhythms
- Reduces symptoms of insomnia and sleep apnea
Benefits for Mental Health
- Releases endorphins and improves mood
- Reduces symptoms of depression and anxiety
- Builds stress resilience
- Improves self-esteem and body image
- Provides social connection (group activities)
Guidelines
- Aim for 150 minutes of moderate exercise per week
- Morning or afternoon exercise is best for sleep
- Avoid vigorous exercise within 3 hours of bedtime
- Even light activity (walking) provides benefits
- Consistency matters more than intensity
Looking Forward: Research and Hope
Research continues to deepen our understanding of the sleep-mental health connection:
Emerging Findings
- Sleep manipulation as a treatment for depression
- The role of specific sleep stages in emotional processing
- Genetic factors influencing both sleep and mental health
- The impact of circadian rhythm disruption on mood disorders
New Treatment Approaches
- Digital CBT-I programs increasing access to treatment
- Targeted memory reactivation during sleep
- Chronotherapy (manipulating sleep timing) for depression
- Integration of sleep treatment into standard mental health care
Conclusion
The interconnection between sleep and mental health is undeniable and profound. They exist in a constant dialogue—each influencing and being influenced by the other. This means that neglecting either one puts both at risk. But it also means that improving either one creates positive ripple effects for the other.
If you’re struggling with sleep, mental health challenges, or both, know that effective treatments exist. The cycle can be broken. Small, consistent changes to sleep habits can improve mental well-being, and addressing mental health can restore restful sleep.
Start with one or two manageable changes. Be patient—it takes time for new habits to show results. And don’t hesitate to seek professional help if you’re struggling. Your sleep and mental health are too important to leave to chance.
Related Resources:
- Pittsburgh Sleep Quality Index (PSQI): Assess your overall sleep quality
- Epworth Sleepiness Scale: Measure your daytime sleepiness
- The Science of Sleep: Understand sleep fundamentals
- Techniques to Fall Asleep Faster: Evidence-based strategies for better sleep onset
- Guide to Common Sleep Disorders: Learn about conditions that disrupt sleep