· Updated: · GoodSleep Team · science-of-sleep · 15 min read
Guide to Common Sleep Disorders: Symptoms, Causes, & Management
Introduction
Sleep disorders affect millions of people worldwide, yet many go undiagnosed or untreated for years—sometimes decades. These conditions can significantly impact every aspect of life: physical health, mental well-being, relationships, work performance, and overall quality of life.
The good news is that most sleep disorders are treatable once properly identified. Understanding the signs and symptoms of common sleep disorders is the first step toward finding effective treatment and reclaiming restorative sleep.
This comprehensive guide covers the most prevalent sleep disorders, their symptoms, causes, diagnostic approaches, and evidence-based management strategies.
For a deeper understanding of how sleep works and its impact on your overall health, explore our Ultimate Guide to Sleep Cycles.
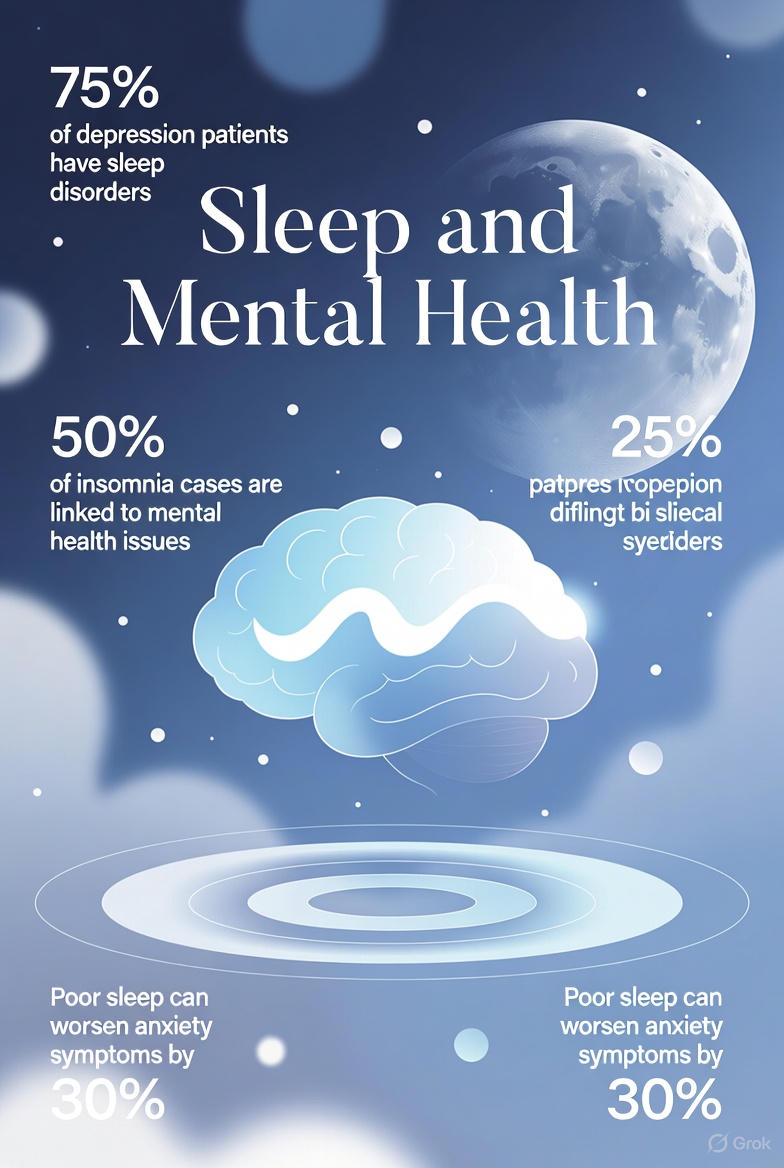
The Prevalence of Sleep Disorders
Sleep disorders are far more common than many people realize:
- 70 million Americans suffer from chronic sleep disorders
- 1 billion people worldwide are estimated to have obstructive sleep apnea
- 30-35% of adults report short-term insomnia symptoms
- 10% of adults have chronic insomnia disorder
- Only 20% of people with sleep apnea have been diagnosed
- Sleep disorders cost the U.S. economy an estimated $411 billion annually in lost productivity
Despite their prevalence, sleep disorders remain underdiagnosed. Many people assume their symptoms are normal or simply a consequence of aging, stress, or a busy lifestyle. Others are unaware that effective treatments exist.
Common Types of Sleep Disorders
Sleep disorders are broadly classified into several categories:
- Insomnias – Difficulty falling or staying asleep
- Sleep-related breathing disorders – Breathing abnormalities during sleep
- Central disorders of hypersomnolence – Excessive daytime sleepiness
- Circadian rhythm sleep-wake disorders – Misalignment of internal clock and environment
- Parasomnias – Abnormal behaviors during sleep
- Sleep-related movement disorders – Movements that interfere with sleep
Let’s explore the most common conditions in detail.
1. Insomnia
Insomnia is the most common sleep disorder, characterized by difficulty falling asleep, staying asleep, or waking up too early without being able to return to sleep—despite adequate opportunity for sleep.
Types of Insomnia
Acute (Short-term) Insomnia:
- Lasts from a few days to a few weeks
- Usually triggered by stress, life changes, or illness
- Often resolves on its own when the trigger passes
Chronic Insomnia:
- Occurs at least 3 nights per week for 3 months or longer
- May have started with an acute trigger but persists due to behavioral and psychological factors
- Requires intervention to resolve
Onset Insomnia:
- Difficulty falling asleep at the beginning of the night
- Often associated with anxiety or racing thoughts
Maintenance Insomnia:
- Difficulty staying asleep or returning to sleep after waking
- Common in depression and some medical conditions
Early Morning Awakening:
- Waking much earlier than intended without being able to return to sleep
- Often associated with depression
Symptoms
- Taking more than 30 minutes to fall asleep
- Waking up frequently during the night (2+ times)
- Waking up too early (2+ hours before intended)
- Sleep that feels unrefreshing despite adequate duration
- Daytime fatigue, low energy, or sleepiness
- Difficulty concentrating or memory problems
- Mood disturbances (irritability, anxiety, depression)
- Worry or frustration about sleep
- Impaired work, school, or social functioning
Causes and Risk Factors
Predisposing factors (make you vulnerable):
- Genetic tendency toward light sleep or anxiety
- Female sex (insomnia is 1.5x more common in women)
- Older age
- Personal or family history of insomnia
Precipitating factors (trigger insomnia):
- Life stress (work, relationships, health, finances)
- Major life transitions (new baby, job change, bereavement)
- Illness or pain
- Changes in sleep environment or schedule
- Medication changes
Perpetuating factors (maintain insomnia):
- Poor sleep habits (irregular schedule, too much time in bed)
- Unhelpful beliefs about sleep (“I must get 8 hours”)
- Compensatory behaviors (napping, sleeping in, using alcohol)
- Conditioned arousal (anxiety about going to bed)
- Caffeine or stimulant use
Management Strategies
Cognitive Behavioral Therapy for Insomnia (CBT-I):
CBT-I is the gold-standard, first-line treatment for chronic insomnia—recommended before medication by major medical organizations.
Components include:
- Sleep restriction: Limiting time in bed to match actual sleep time, then gradually expanding
- Stimulus control: Strengthening the bed-sleep association; leaving bed if unable to sleep
- Cognitive restructuring: Challenging unhelpful thoughts about sleep
- Sleep hygiene education: Optimizing behaviors and environment
- Relaxation training: Progressive muscle relaxation, breathing exercises
Effectiveness: 70-80% of patients show significant improvement, with effects maintained long-term.
Medications:
- Z-drugs (zolpidem, eszopiclone): Short-term use only; risk of dependence
- Low-dose sedating antidepressants (trazodone, doxepin): May help with maintenance
- Melatonin receptor agonists (ramelteon): Help with sleep onset
- Orexin receptor antagonists (suvorexant, lemborexant): Newer option for onset and maintenance
Important: Medications should be used cautiously and typically in combination with behavioral approaches. Long-term use of hypnotics is not recommended.
2. Sleep Apnea
Sleep apnea involves repeated interruptions in breathing during sleep, leading to fragmented sleep, oxygen desaturation, and numerous health consequences.
Types of Sleep Apnea
Obstructive Sleep Apnea (OSA):
- The most common form (84% of cases)
- Caused by physical blockage of the airway when throat muscles relax
- Breathing resumes with a snort or gasp when the brain arouses briefly
Central Sleep Apnea (CSA):
- The brain temporarily fails to signal breathing muscles
- No physical obstruction; respiratory effort is absent
- Often associated with heart failure, stroke, or opioid use
Complex (Treatment-Emergent) Sleep Apnea:
- Begins as OSA but central events appear during CPAP treatment
- May require specialized therapy like ASV
Symptoms
Nighttime symptoms:
- Loud, chronic snoring (often first noticed by a bed partner)
- Witnessed breathing pauses (apneas)
- Gasping, choking, or snorting during sleep
- Restless sleep and frequent position changes
- Frequent nighttime urination (nocturia)
- Night sweats
- Dry mouth upon awakening
Daytime symptoms:
- Excessive daytime sleepiness
- Morning headaches
- Difficulty concentrating or memory problems
- Mood changes (irritability, depression, anxiety)
- Decreased libido
- Fatigue that doesn’t improve with more sleep
Risk Factors
For OSA:
- Excess body weight (strongest modifiable risk factor)
- Large neck circumference (>17” men, >16” women)
- Male sex (2-3x higher risk than women)
- Age (risk increases with age)
- Family history
- Anatomical factors (large tonsils, recessed chin, deviated septum)
- Alcohol and sedative use
- Smoking
- Nasal congestion
For CSA:
- Heart failure
- Stroke
- Opioid use
- High altitude
- Certain medications
Health Consequences of Untreated Sleep Apnea
Sleep apnea is not just a sleep problem—it’s a systemic health condition:
| System | Consequences |
|---|---|
| Cardiovascular | Hypertension, heart disease, arrhythmias, stroke |
| Metabolic | Insulin resistance, type 2 diabetes, weight gain |
| Cognitive | Memory impairment, concentration problems, dementia risk |
| Mental Health | Depression, anxiety, mood instability |
| Safety | Drowsy driving accidents, workplace injuries |
| Quality of Life | Fatigue, reduced productivity, relationship strain |
For more on these risks, see Dangers of Untreated Sleep Apnea.
Diagnosis
Polysomnography (PSG): Overnight sleep study in a lab monitoring brain activity, eye movements, muscle tone, heart rate, breathing, and oxygen levels.
Home Sleep Apnea Testing (HSAT): Simplified testing at home that monitors breathing, oxygen, and sometimes heart rate. Suitable for patients with high likelihood of moderate-to-severe OSA.
Key metric: Apnea-Hypopnea Index (AHI) = breathing events per hour
- Normal: <5
- Mild OSA: 5-15
- Moderate OSA: 15-30
- Severe OSA: >30
Management Strategies
Continuous Positive Airway Pressure (CPAP):
- Gold standard treatment for moderate-to-severe OSA
- A mask delivers pressurized air to keep the airway open
- Highly effective when used consistently
- Learn more in our CPAP Beginner’s Guide
Other PAP devices:
- BiPAP: Two pressure levels (higher for inhale, lower for exhale)
- APAP: Auto-adjusting pressure based on detected events
- ASV: Adaptive servo-ventilation for central/complex apnea
Oral appliances:
- Mandibular advancement devices reposition the jaw to keep the airway open
- Better tolerated than CPAP for some patients
- Typically used for mild-to-moderate OSA
Surgical options:
- UPPP (uvulopalatopharyngoplasty): Removes excess tissue
- Inspire therapy: Implanted device stimulates hypoglossal nerve
- Maxillomandibular advancement: Repositions jaw bones
- Tonsillectomy/adenoidectomy: Especially in children
Lifestyle modifications:
- Weight loss (even 10% can significantly improve AHI)
- Positional therapy (avoiding back sleeping)
- Avoiding alcohol and sedatives before bed
- Treating nasal congestion
- Smoking cessation
3. Restless Legs Syndrome (RLS)
Restless Legs Syndrome creates an irresistible urge to move the legs, often accompanied by uncomfortable sensations. It typically occurs in the evening or at night, significantly interfering with sleep.
Symptoms
Primary symptoms (all must be present for diagnosis):
- An urge to move the legs, usually accompanied by uncomfortable sensations
- Symptoms begin or worsen during rest or inactivity
- Symptoms are partially or totally relieved by movement
- Symptoms worsen in the evening or night
Description of sensations:
- Crawling, creeping, pulling, or tugging
- Itching or tingling deep in the legs
- “Electric” or buzzing sensations
- Aching or throbbing
- Often described as difficult to put into words—not typical pain
Associated features:
- Difficulty falling asleep due to symptoms
- Periodic limb movements during sleep (PLMS)—involuntary leg jerks that fragment sleep
- Daytime fatigue and sleepiness
- Difficulty sitting still (movies, flights, meetings)
Types of RLS
Primary (Idiopathic) RLS:
- No identifiable underlying cause
- Often runs in families
- May begin at any age but typically worsens over time
Secondary RLS:
- Caused by or associated with another condition:
- Iron deficiency (most common)
- Kidney disease/dialysis
- Pregnancy (usually resolves after delivery)
- Peripheral neuropathy
- Parkinson’s disease
- Certain medications (antidepressants, antihistamines, anti-nausea drugs)
Management Strategies
Address underlying causes:
- Check and correct iron deficiency (ferritin <50-75 ng/mL may worsen RLS)
- Review medications that may exacerbate symptoms
- Manage associated conditions
Lifestyle modifications:
- Regular moderate exercise (but not close to bedtime)
- Leg stretching before bed
- Warm baths or massage
- Hot or cold packs to legs
- Reducing caffeine, alcohol, and nicotine
- Good sleep hygiene
Medications:
- Dopamine agonists (pramipexole, ropinirole): First-line for moderate-to-severe RLS, but risk of augmentation with long-term use
- Alpha-2-delta ligands (gabapentin, pregabalin): Increasingly preferred due to lower augmentation risk
- Low-dose opioids (for refractory cases)
- Iron supplementation (if ferritin is low)
4. Narcolepsy
Narcolepsy is a chronic neurological disorder affecting the brain’s ability to regulate sleep-wake cycles. It causes overwhelming daytime sleepiness and, in some cases, sudden muscle weakness triggered by emotions.
Types of Narcolepsy
Type 1 Narcolepsy (with cataplexy):
- Characterized by excessive daytime sleepiness plus cataplexy
- Caused by loss of neurons that produce hypocretin (orexin)
- Usually develops in adolescence or young adulthood
Type 2 Narcolepsy (without cataplexy):
- Excessive daytime sleepiness without cataplexy
- Hypocretin levels are usually normal
- Less well understood
Symptoms
Excessive daytime sleepiness (EDS):
- The hallmark symptom—present in all cases
- Persistent, overwhelming sleepiness despite adequate nighttime sleep
- “Sleep attacks”—irresistible urges to sleep, even in inappropriate situations
- Brief naps are often refreshing but sleepiness returns within hours
Cataplexy (Type 1 only):
- Sudden, brief loss of muscle tone triggered by strong emotions
- Triggers include laughter, surprise, anger, or excitement
- Can range from slight weakness (drooping eyelids, head drop) to complete collapse
- Person remains conscious during episodes
- Episodes last seconds to minutes
Sleep paralysis:
- Temporary inability to move or speak when falling asleep or waking up
- Can be frightening but is not dangerous
- Lasts seconds to minutes
Hypnagogic/hypnopompic hallucinations:
- Vivid, dream-like experiences when falling asleep or waking
- Often visual but can be auditory or tactile
- Can be disturbing or frightening
Disrupted nighttime sleep:
- Despite excessive sleepiness, nighttime sleep is often fragmented
- Frequent awakenings and vivid dreams
Management Strategies
Lifestyle modifications:
- Scheduled short naps (10-20 minutes, 2-3 times daily)
- Regular sleep schedule
- Good sleep hygiene
- Avoiding alcohol and heavy meals
- Regular exercise
- Safety planning (driving, operating machinery)
Medications for excessive sleepiness:
- Modafinil/armodafinil: Wake-promoting agents; first-line treatment
- Sodium oxybate (Xyrem/Xywav): Also helps cataplexy; taken at night
- Pitolisant: Newer histamine-3 receptor antagonist
- Solriamfetol: Newer dopamine/norepinephrine reuptake inhibitor
- Traditional stimulants: Amphetamines, methylphenidate (second-line)
Medications for cataplexy:
- Sodium oxybate
- Antidepressants (SSRIs, SNRIs, TCAs)
- Pitolisant
Support:
- Education about the condition
- Support groups
- Workplace accommodations
- Counseling for emotional impact
5. Circadian Rhythm Sleep-Wake Disorders
These disorders occur when your internal biological clock (circadian rhythm) is misaligned with your external environment or social demands.
Delayed Sleep-Wake Phase Disorder (DSWPD)
What it is: A pattern of falling asleep and waking up much later than conventional times—often going to bed after 2 AM and waking after 10 AM.
Who it affects: Most common in adolescents and young adults.
Symptoms:
- Unable to fall asleep at conventional bedtimes
- Extremely difficulty waking in the morning
- Daytime sleepiness when forced to wake early
- Normal sleep quality and duration when allowed to follow preferred schedule
Management:
- Light therapy in the morning
- Avoiding bright light in the evening
- Melatonin 0.5-3mg, 5-7 hours before natural sleep time
- Gradual schedule advancement (chronotherapy)
- Consistent wake times even on weekends
Advanced Sleep-Wake Phase Disorder (ASWPD)
What it is: Falling asleep and waking much earlier than desired—often sleeping 7-9 PM and waking 3-5 AM.
Who it affects: More common in older adults.
Management:
- Light therapy in the evening
- Avoiding morning bright light
- Social activities in the evening to promote later bedtime
Shift Work Sleep Disorder
What it is: Insomnia and/or excessive sleepiness due to working night shifts or rotating shifts.
Prevalence: Affects 10-40% of shift workers.
Symptoms:
- Difficulty sleeping during daytime hours
- Excessive sleepiness during night shifts
- Reduced total sleep time (1-4 hours less than day workers)
- Increased accident risk
- Gastrointestinal problems
Management:
- Strategic napping before and during shifts
- Light therapy during night shifts
- Dark, quiet sleep environment for daytime sleep
- Consistent shift schedule when possible
- Melatonin to promote daytime sleep
- Caffeine strategically (not too close to sleep time)
Jet Lag Disorder
What it is: Temporary sleep disruption when traveling across multiple time zones.
Symptoms:
- Difficulty sleeping at the new local time
- Daytime sleepiness and fatigue
- Difficulty concentrating
- Gastrointestinal symptoms
Management:
- Pre-adaptation: Gradually shift schedule before travel
- Light exposure: Seek or avoid light based on travel direction
- Melatonin: Take at new local bedtime
- Stay hydrated and avoid alcohol
- Short naps if needed (but not too close to bedtime)
6. Parasomnias
Parasomnias are abnormal behaviors, movements, emotions, or perceptions that occur during sleep or sleep-wake transitions.
NREM Parasomnias (Disorders of Arousal)
Sleepwalking (Somnambulism):
- Walking or performing complex behaviors while asleep
- Eyes may be open but person is not aware
- Can range from sitting up in bed to leaving the house
- Usually occurs in first third of night (during deep sleep)
- More common in children; most outgrow it
Sleep Terrors (Night Terrors):
- Episodes of intense fear, screaming, and agitation during sleep
- Person appears terrified but is not fully awake
- Usually no memory of the episode
- Most common in children
Confusional Arousals:
- Confused, disoriented behavior when waking from deep sleep
- May include inappropriate speech or slow responses
- Common in children and those who are sleep-deprived
Management of NREM parasomnias:
- Ensure adequate sleep (deprivation is a trigger)
- Maintain regular sleep schedule
- Safety measures (locking doors, removing obstacles)
- Avoid alcohol and certain medications
- Treat underlying sleep disorders (especially sleep apnea)
- Medications (benzodiazepines) in severe cases
REM Sleep Behavior Disorder (RBD)
What it is: Acting out dreams during REM sleep due to failure of normal muscle paralysis (atonia).
Symptoms:
- Talking, yelling, or shouting during sleep
- Punching, kicking, or other violent movements
- May cause injury to self or bed partner
- Can recall vivid, often violent dreams if awakened
Important: RBD can be an early sign of neurodegenerative disorders (Parkinson’s, Lewy body dementia). Patients should be monitored long-term.
Management:
- Safety measures (padded bed rails, mattress on floor)
- Remove dangerous objects from bedroom
- Melatonin (3-12mg at bedtime)
- Clonazepam if melatonin insufficient
Nightmare Disorder
What it is: Recurring disturbing dreams that cause significant distress or impair functioning.
Management:
- Address underlying stress, trauma, or anxiety
- Image Rehearsal Therapy: Rewrite nightmare ending while awake, rehearse new version
- Prazosin (especially for PTSD-related nightmares)
- Good sleep hygiene
Recognizing When to Seek Help
Many people live with sleep problems for years without realizing they have a treatable condition. Consider seeking evaluation if you experience:
Warning Signs
- Sleep problems lasting more than 3-4 weeks
- Excessive daytime sleepiness affecting work, driving, or safety
- Loud snoring, especially with witnessed pauses or gasping
- Difficulty falling or staying asleep despite opportunity
- Uncomfortable leg sensations that worsen at rest
- Unusual behaviors during sleep
- Falling asleep at inappropriate times
- Persistent fatigue despite adequate time in bed
When to Consult a Healthcare Professional
- Sleep issues significantly impact quality of life
- Self-help strategies haven’t worked after 2-3 weeks
- You’ve fallen asleep while driving or in other dangerous situations
- A bed partner reports concerning symptoms (apneas, movements, behaviors)
- You’re concerned about symptoms even if they seem minor
Diagnostic Process
Clinical Evaluation
A healthcare provider will typically:
- Take a detailed sleep history
- Review medical history and medications
- Perform a physical examination
- Ask about family history
- Use standardized questionnaires
Sleep Studies
Polysomnography (PSG):
- Comprehensive overnight study in a sleep laboratory
- Monitors brain waves (EEG), eye movements (EOG), muscle activity (EMG), heart rhythm (ECG), breathing, and oxygen levels
- Gold standard for diagnosing sleep apnea, narcolepsy, parasomnias, and other disorders
Home Sleep Apnea Testing (HSAT):
- Simplified testing done at home
- Monitors breathing, oxygen, and sometimes heart rate
- Appropriate for patients with high suspicion of uncomplicated OSA
Multiple Sleep Latency Test (MSLT):
- Series of 4-5 daytime naps to measure sleep tendency
- Used to diagnose narcolepsy and idiopathic hypersomnia
- Measures how quickly you fall asleep and whether you enter REM
Maintenance of Wakefulness Test (MWT):
- Measures ability to stay awake in a quiet, dimly lit environment
- Used to assess treatment effectiveness or safety (e.g., for drivers)
Self-Assessment Tools
Before seeing a specialist, validated questionnaires can help assess your symptoms:
- Epworth Sleepiness Scale (ESS): Measures daytime sleepiness
- Pittsburgh Sleep Quality Index (PSQI): Assesses overall sleep quality
- OSA Risk Assessment Quiz: Screens for obstructive sleep apnea risk
- Insomnia Severity Index (ISI): Measures insomnia severity
Treatment Approaches Overview
Behavioral Treatments
- CBT-I: For insomnia—restructuring thoughts and behaviors
- Sleep hygiene education: Optimizing habits and environment
- Relaxation techniques: Progressive muscle relaxation, breathing exercises
- Stimulus control: Strengthening the bed-sleep association
- Sleep restriction: Consolidating sleep by limiting time in bed
- Image rehearsal therapy: For nightmares
Medical Treatments
- Prescription medications: Specific to each disorder
- Medical devices: CPAP, BiPAP, oral appliances
- Surgery: For specific cases of sleep apnea or structural issues
- Supplements: Melatonin, iron (when indicated)
- Light therapy: For circadian rhythm disorders
Lifestyle Modifications
- Weight management (especially for sleep apnea)
- Regular exercise (but not too close to bedtime)
- Dietary changes (limiting caffeine, alcohol, heavy meals)
- Stress management techniques
- Sleep schedule optimization
Sleep Diary: A Valuable Tool
Keeping a sleep diary for 1-2 weeks before seeing a healthcare provider provides valuable information:
What to Track
| Time/Event | Details |
|---|---|
| Bedtime | When you got into bed |
| Sleep onset | Estimated time you fell asleep |
| Awakenings | Number, duration, and reason (if known) |
| Wake time | When you woke for the day |
| Rise time | When you got out of bed |
| Sleep quality | Rating (1-10) of how you feel |
| Daytime naps | Time and duration |
| Caffeine | Amount and timing |
| Alcohol | Amount and timing |
| Medications | Sleep-related and otherwise |
| Exercise | Type and timing |
| Symptoms | Snoring, leg discomfort, nightmares, etc. |
The Impact of Untreated Sleep Disorders
Health Consequences
- Cardiovascular: Hypertension, heart disease, stroke, arrhythmias
- Metabolic: Obesity, diabetes, metabolic syndrome
- Immune: Weakened immune function, increased infection risk
- Mental Health: Depression, anxiety, cognitive decline
- Neurological: Increased dementia risk, impaired memory
Safety Concerns
- Motor vehicle accidents: Drowsy driving is as dangerous as drunk driving
- Workplace accidents: Reduced alertness and slowed reactions
- Medical errors: Healthcare workers with sleep disorders make more errors
- Falls: Especially in older adults with sleep disruption
Quality of Life
- Reduced productivity and performance
- Strained relationships
- Decreased enjoyment of activities
- Lower overall life satisfaction
Support and Resources
Professional Organizations
- American Academy of Sleep Medicine (AASM): aasm.org
- National Sleep Foundation: thensf.org
- American Sleep Apnea Association: sleepapnea.org
- Restless Legs Syndrome Foundation: rls.org
- Narcolepsy Network: narcolepsynetwork.org
Finding a Sleep Specialist
- Ask your primary care physician for a referral
- Search the AASM’s sleep center directory
- Look for board-certified sleep medicine physicians
- Consider both in-person and telemedicine options
Conclusion
Sleep disorders are common but treatable conditions that can significantly impact every aspect of life. The key is recognition—understanding that chronic sleep problems are not something to simply “push through” or accept as normal.
If you’re struggling with sleep, take these steps:
- Track your symptoms with a sleep diary
- Take validated self-assessment questionnaires
- Discuss concerns with a healthcare provider
- Seek specialist evaluation if indicated
- Commit to recommended treatments
With proper diagnosis and treatment, most people with sleep disorders can achieve dramatic improvements in their sleep quality, daytime functioning, and overall health. Restorative sleep is not a luxury—it’s a biological necessity. You deserve to get the rest you need.
Ready to assess your sleep health?
- Pittsburgh Sleep Quality Index (PSQI): Evaluate your overall sleep quality
- Epworth Sleepiness Scale (ESS): Measure your daytime sleepiness
- OSA Risk Assessment Quiz: Screen for obstructive sleep apnea
- Sleep Cycle Calculator: Optimize your sleep timing
For more information on specific topics, explore our Sleep Science category or learn about The Science of Sleep.